In this Post you will be able to take quiz containing important MCQs of Oral and Maxillofacial Surgery and topic covered in this Quiz will be Mandibular Fractures and Middle Third of Face Fractures. Correct Answers are Marked in Bold and Blue colour.
-
- Patient with maxillofacial injuries should be carried in:
A. Supine position
B. Lateral position
C. Prone position
D. Sitting position - The presence of tension pneumothorax should be considered in patients who has feature as:
A. Development of severe respiratory distress with decreased breath sounds, hyper resonance on one side of chest
B. Development of severe respiratory distress and deviation of trachea to the side involved
C. Patient becomes acutely ill, with collapsed neck veins.
D. All of the above - Raised intracranial pressure following a maxillofacial injury, is:
A. Normal finding
B. Typically associated with an increase in the heart rate
C. Typically associated with an increase in the blood pressure
D. Usually subsides spontaneously - Which of the following is an immediate danger to a patient with severe
facial Injuries
A. Bleeding
B. Associated fracture spine
C. Infection
D. Respiratory obstruction
- Which of the following always indicates obstruction to the airway?
A. Slow pounding pulse
B. Stertorous breathing
C. Increase in pulse rate
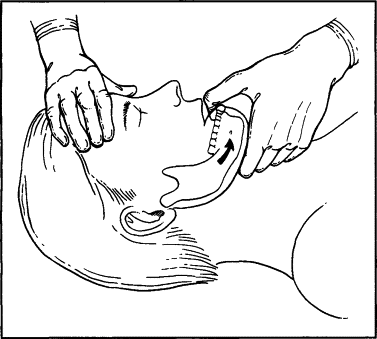
D. Decrease in blood pressure - The head tilt procedure while dealing with an unconscious patient in dental chair is done to ensure
A. Patent airway
B. Blood circulation to the brain
C. To clear the foreign body obstacle
D. To relieve spasm of respiratory muscles - Of the following, which is the immediate treatment for a patient with
comminuted fracture and in the state of shock?
A. Ringer’s lactate solution by IV route
B. Normal saline by IV route
C. Blood transfusion
D. Plasma expanders - Definitive management of maxillofacial trauma after trauma can be delayed up to what time without substantially compromising the outcome?
A. Should be done 5-7 days of admission
B. Can be delayed up to 2 weeks
C. Should be performed immediately after admission
D. None - Clinical sign that is always positive in bone fracture is
A. Crepitus
B. Tenderness
C. Abnormal mobility
D. All of the above - Direct impact on the bone will produce a
A. Transverse fracture
B. Oblique fracture
C. Spiral fracture
D. Comminuted fracture - Green stick fractures are most common with a…………
A. Older people
B. Adult
C. Children
D. Soldiers - Osteomyelitis is most commonly associated with…………
A. Compound fractures
B. Comminuted fractures
C. Green stick fractures
D. Telescopic fracture - Principles in treating fractures include
A. Reduction of fracture
B. Fixation of fracture and restoration of occlusion
C. Immobilization
D. All of the above
- During panfacial fractures the structures that are reconstructed first are
A. Outer bone segments of the frame
B. Bones inside the framework
C. Maxilla always
D. Mandible always - The most common site of fracture of the mandible is the:
A. Body
B. Angle
C. Symphysis
D. Condyle - The weakest part and most vulnerable part for fracture in the mandible is:
A. Ramus of mandible
B. Condylar neck
C. Angle of the mandible
D. Region of the canine tooth - Bones usually fracture at the site of:
A. Compressive strain
B. Tensile strain
C. Rich blood supply
D. Thin periosteal covering - Orbital blow out fracture is best seen in?
A. Reverse town
B. Waters view
C. PA view
D. Submentovertex - The radiographic view of choice for diagnosing horizontally favorable/unfavorable # is:
A. OPG
B. Occlusal
C. Lateral Oblique view
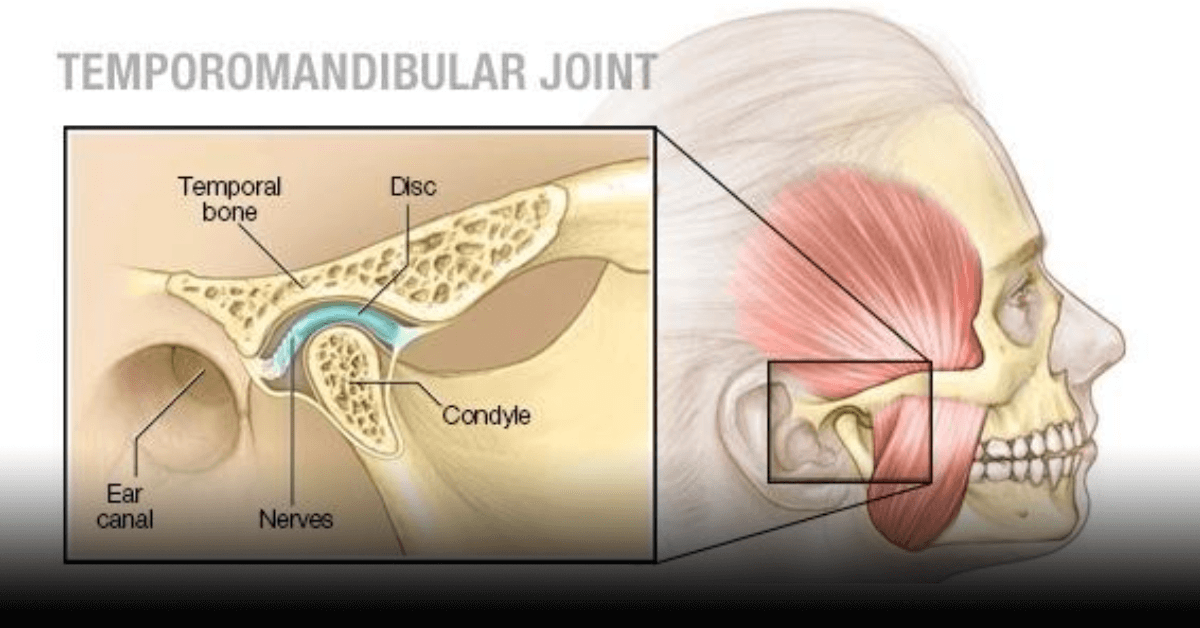
D. Transpharyngeal - Condylar neck fracture best detected in:
A. Submentovertex projection
B. Water’s projection
C. Posterio anterior skull projection
D. Reverse towne projection
- Of the following which is almost pathognomonic of a mandibular fracture:
A. Deep laceration near the area of trauma and paresthesia
B. Ecchymosis in the lingual sulcus and dearranged occlusion
C. Anterior open bite and deviation of the mandible on opening
D. None of the above are correct. There is no pathogenic feature of mandibular fracture - All are features of mandibular fracture except:
A. Malocclusion
B. Paresthesia of lower lip
C. Fractured ends are prevented from dislocation by masticatory muscles
D. Are usually compound - The proximal segment of mandible angle fracture usually displaced in:
A. Anterior and superior
B. Posterior and interior
C. Interior only
D. Posterior and superior - In a patient with bilateral dislocated fractures of the necks of the mandibular condyles, one can expect the following clinical signs
A. Anterior open bite
B. Inability to protrude the mandible
C. Inability to bring posterior molars into contact
D. A & B
- Which of the following are most complicated fractures?
A. Symphysis
B. Body
C. Condyle
D. Angle - A 7-year-old boy presented with fracture of left sub condylar region with occlusion undisturbed, the treatment would be:
A. Immobilization for 7 day
B. Immobilization for 14 days with intermittent active opening
C. No immobilization with restricted mouth opening for 10 days
D. No immobilization and no active treatment
- In children fracture mandible which has not been perfectly reduced but has become firm with slight imperfection, the choice of the management would be:
A. Arch bar and elastric traction
B. Accept the slight imperfection and allow for later remodeling
C. Refracture and plating
D. Refracture and interosseous wiring - An adult patient sustained a subcondylar fracture on the left side. Clinically it is seen that there is
A. Moderate intraoral bleeding
B. Trismus and bilateral crepitus
C. Deviation of the mandible to the right-on protrusion
D. Inability to deviate the mandible to the right-on opening
- The muscle, under the influence of which, the superior fragment of condyle, in a condylar neck # is displaced anteriorly and medially is:
A. Medial Pterygoid
B. Lateral Pterygoid
C. Masseter
D. Temporalis - In case of pure symphysis fracture of mandible, fracture segments are usually displaced
A. Lingually & downward by the pull of Genioglossus mylohyoid muscles.
B. Mainly lingually and lingual & downward movement due to the pull of Geniohyoid & myohyoid muscle.
C. Mainly upward movement. Lingual and upward movement due to the pull of Geniohyoid and mylohyoid muscle.
D. None of the above are correct. A little (or) no displacement occurs.
- Posterior displacement of the fractured anterior segment in the bilateral fracture of the mandible in the canine region is due to the action of the
A. Thyrohyoid, genioglossus and geniohyoid
B. Mylohyoid, genioglossus and geniohyoid
C. Geniohyoid and genioglossus and anterior belly of digastric muscles
D. Mylohyoid, geniohyoid and thyrohyoid muscle - A fractured coronoid process of mandible displaces upwards by the action of following muscle
A. Buccinator
B. Lateral Pterygoid
C. Mylohyoid
D. Temporalis
- Which of the following is seen with guardsman fracture associated with bilateral condylar fractures
A. Increased intercanthal distance
B. Increased interpupillary distance
C. Increased gonion gnathion distance
D. Increased interangular distance
- Fracture most commonly resulting in widening of face is?
A. Parasymphyseal and symphyseal region fracture without condylar fracture
B. Parasymphyseal and symphyseal region fracture with condylar fracture
C. Zygomaticomaxillary complex fracture
D. Cranio-facial disjunction fracture - Fracture of mandible not involving dental arch is treated by
A. Open reduction
B. Closed reduction
C. No treatment required
D. None of the above - A displaced, unfavorable fracture in the mandibular angle region is a potentially difficult fracture to treat because of:
A. Injury to neurovascular bundle
B. Malocclusion secondary to injury
C. Distraction of fracture segments by muscle pull
D. Increased density of bone in this region of mandible - Unfavorable fracture of angle of mandible is best treated by:
A. Closed reduction with IMF
B. Closed reduction with cap splint
C. Open reduction with bone plate fixation
D. Circummandibular wiring - The splint which is most commonly used in dentulous mandibular fracture is:
A. Gunning splint
B. Cap splint
C. Ribbon splint
D. All of these - How many weeks of fixation are required for fracture mandible?
A. 8-10 weeks
B. 6-8 weeks
C. 4-6 weeks
D. 2-4 weeks - Which of the following is used for ‘figure of eight’ wiring for stabilization of subluxated teeth in alveolar injuries?
A. 0.23 mm stainless steel wire
B. 0.35 mm stainless steel wire
C. 0.45 mm stainless steel wire
D. 0.55 mm stainless steel wire - A fracture of the mandible in the canine region in a 6-year-old child should be managed by:
A. Cap splint fixation
B. Intermaxillary fixation
C. Risdon wiring
D. Transosseous wiring - Which one of the following is not an appropriate method of stabilizing # in childhood
A. Arch bar with circumdental wiring
B. Circumdental wiring with skeletal wiring
C. Risdon wiring
D. Splints - The movement employed in the reduction of dislocated non-fractured mandible condyle is:
A. Downward and backward
B. Upward and forward
C. Upward and backward
D. Downward and forward - Paresthesia is one of the commonest finding in which of the following fractures?
A. Subcondylar fracture of the mandible
B. Zygomatico maxillary complex fracture
C. Fractured coronoid and displacement of the fracture
D. Symphysis fracture associated with bilateral subcondylar fracture - Paresthesia over nasal and upper lip following fractured zygoma is because of involvement of
A. Facial nerve
B. Posterior superior alveolar nerve
C. Infraorbital nerve
D. Mental nerve - A 35-year-old man with a Le Fort III fracture complains of blood tinged watery discharge from his nose 2 days after the trauma. CT scan confirms NOE fracture as well. What clinical features suggest that the discharge is CSF Leak?
A. Continuous discharge
B. Appearance of tram line or halo rings
C. Stoppage of discharge on pressure
D. None of the above - The most common site of leak in CSF rhinorrhoea is
A. Sphenoid sinus
B. Frontal sinus
C. Cribriform plate
D. Tegmen tympani - CSF rhinorrhea is not seen in
A. Le Fort I
B. Le Fort II
C. Le Fort III
D. Ethmoidal - Le Fort III fracture is the same as
A. Craniofacial disjunction
B. Guerrin’s fracture
C. Pyramidal fracture
D. None of the above - Floating maxilla is typically found in
A. Le Fort I or Guerin fractures
B. Le Fort II or pyramidal fractures
C. Craniomandibular dysjunction
D. All of the above - In Le Fort I fracture, the fracture fragment includes all of the following except the:
A. Bridge of the nose
B. Nasal spine
C. Lower portions of the pterygoid
D. Upper teeth and palate processes - Which of the following is characteristic of Le Fort I fracture?
A. CSF rhinorrhea
B. Bleeding from the ear
C. Bleeding into the antrum
D. A & B - “Panda Facies” is one of the term to describe the patient’s face after mid face trauma. The appearance is due to:
A. Gross swelling of the face
B. C.S.F. rhinorrhea and bleeding from the nose & laceration results in red &
white streaks on the face
C. Edema & ecchymosis around the eyes
D. Sub-conjunctival hemorrhage (bilateral) - The Sub-conjunctival hemorrhage remains red in color for a long time because?
A. Hemoglobin prevents breakdown of R.BC.
B. Permeability of the conjunctiva to oxygen
C. Oxygen content of blood to conjunctiva is vey high
D. All of the above - Bilateral subconjunctival ecchymosis is not associated with
A. Le Fort II fracture
B. Le-Fort III fracture
C. Naso ethmoidal complex fracture
D. Le-Fort I fracture
- The incision used for treatment of traumatic telecanthus is
A. Bicoronal incision
B. Upper blepheroplasty
C. Infraorbital incision
D. Preauricular incision - In Le Fort III fracture which of the following are seen:
A. Whole face is mobile with crack pot sound on tapping teeth
B. CSF rhinorrhea
C. Fracture at frontozygomatic suture
D. All of the above
- Battle sign is seen in:
A. # of anterior cranial fossa
B. # of middle cranial fossa
C. # of posterior cranial Fossa
D. None of the above - Of the following which is weakest part of orbit:
A. Medial wall
B. Lateral wall
C. Floor of the orbit
D. A&B
E. A&C
- Hanging drop effect in blow-out fracture is due to herniation of
A. Superior oblique and inferior oblique muscles
B. Inferior oblique and inferior rectus muscles
C. Superior rectus and superior oblique muscles
D. Inferior oblique and superior rectus muscle - Diplopia is most common with:
A. Mandibular body fracture
B. Alvedan fractures
C. Craniofacial dysjunction
D. Zygomatico maxillary complex
- After orbital injury the cause of diplopia in the acute phase is?
A. Ischemic injury leading to fibrosis
B. Entrapment of extra ocular muscles
C. Intrusion of eye
D. None of the above - Which of the following statements about a blow-out fracture are true?
A. It has been established beyond doubt that such an injury is caused by the eyeball being forced backwards, thus raising the intraorbital pressure and causing the thin orbital floor to blow-out.
B. If the patient has diplopia and a coronal tomogram shows a small blow-out of the orbital floor, it should be repaired immediately.
C. Early repair of the orbital floor always prevents enophthalmos
D. None of the above
- In a patient with fresh blowout fracture of the orbit, best immediate management is
A. Wait and watch
B. Antral pack
C. Titanium mesh
D. Glass bead mesh - Gillis approach for reduction of zygomatic fracture is done through
A. Temporal fossa
B. Intra temporal fossa
C. Infra orbital fossa
D. All of the above - In depressed zygomatic arch fracture, difficult in opening the mouth is caused by impingement of
A. Condyles
B. Ramus
C. Petrous temporal
D. Coronoid process
- After fracture of middle cranial foramen there is epiphora this is due to damage of
A. Ciliary ganglion
B. Greater palatine nerve
C. Infraorbital nerve
D. Nasolacrimal duct
- All of the following statements of nasal fractures are true except
A. Even if minor, they may be followed by bilateral ecchymosis and facial oedema
B. They may need to be reduced for a few weeks
C. They need not be complicated by traumatic telecanthus
D. They may lead to the telescoping of the nasal complex into the frontal sinus - Which of the following statements about CSF rhinorrhoea is true?
A. It suggests a fracture of the petrous temporal bone
B. It reduces after a Valsalva manoeuvre
C. The fluid tastes sweet
D. None of the above
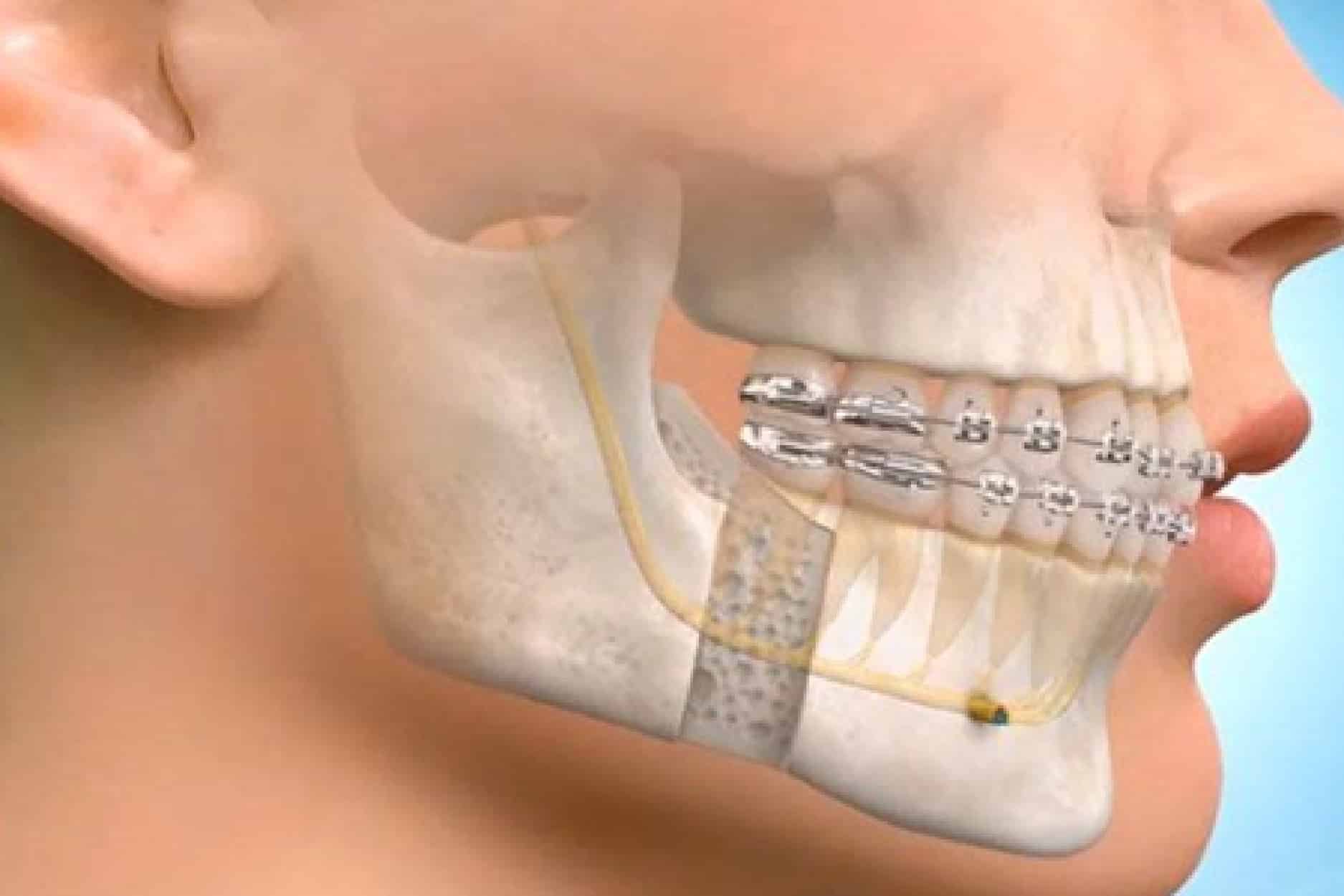
- 70. Which of the following methods of osteosynthesis in the treatment of fracture mandible results in primary bone healing?
A. Mini-plates
B. Intraosseous wiring
C. Inter-maxillary fixation
D. Compression bone plates
- In osteosynthesis all are used except:
A. Lag screw
B. Wires
C. Clampy bone plate
D. Eyelet wiring
- Miniplate fixation is effective at:
A. Zone of tension
B. Near the roots of teeth
C. Zone of compression
D. Near to the mental foramen - Where on a true lag screw are the threads placed?
A. On the distal end, only
B. On the end close to the head
C. On the entire length of screw
D. Both on distal end and the end near the head - In fracture of atrophic mandible treatment modality is
A. Bone grafting & load bearing
B. Bone grafting & load sharing
C. Open reduction
D. Semi rigid - Mandibular fracture managed by adapting mini plates is a type of
A. Load bearing osteosynthesis
B. Load sharing osteosynthesis
C. Non-rigid osteosynthesis
D. Rigid osteosynthesis - Primary healing of a mandibular fracture is seen following fixation with:
A. Gunning splints
B. Compression plates
C. Trans-osseous wires
D. Champy plates - According to the tension and compression forces acting at the condylar border which of these would best attenuate them?
A. A plate at the anterior border and another at the posterior border
B. A plate at the anterior border
C. A plate at the post border
D. A plate at the lateral border
- The optimum length of screw, for fixation of plate in mandible is
A. 2 mm
B. 3 mm
C. 4 mm
D. 6 mm - Open reduction and internal fixation of fracture fragments in the older patients is risky because
A. of their old age, they less likely tolerate the major procedure under general anesthesia.
B. fixation is difficult because bone will become denser as age advances.
C. delayed (or) non-union may occur because of over all decrease in reparative abilities of the body.
D. None of the above are correct.
- Eburnation is seen in:
A. Malunion
B. Non-union
C. Osteomyelitis
D. Osteoradionecrosis - Which of the following is a complication of an open fracture?
A. Malunion
B. Nonunion
C. Infection
D. Crepitation - Cause of death during the 2nd peak in a patient with severe injuries is:
A. Spinal injury
B. Epidural and Subdural hemorrhage
C. Aortic arch rupture
D. Sepsis - A patient with suspendcted cervical fracture should be kept in:
A. Prone position
B. Both body and neck flexed
C. Body and neck extended
D. Body extended and neck flexed - The recommendation about the resuscitation of elderly trauma patients include all except
A. The presence of pre-existing medical conditions will adversely affect the outcome in elderly trauma patient.
B. Elderly trauma patients (65 years or older) with a GCS score less than 8 has a very poor prognosis. If improvement is not possible within 72 hours, then limitation of continued aggressive therapy should be considered.
C. Invasive hemodynamic monitoring is not indicated for those geriatric trauma patients even with uncertain cardiovascular or renal diseases.
D. Effort should be made to optimize the cardiac index (>4 L/min./m2) and oxygen consumption index (170 mL/min/m2) - Gunshot wounds of the face caused by
A. Low-veiocity hand-gun bullets are typically less serious than those caused by high velocity missiles.
B. Low-velocity missiles have a deceptive external appearance in that there is extensive internal damage covered by a small entry wound.
C. High-velocity bullets are sterile.
D. High-velocity bullets must be sutured as soon as possible. - From the scheme given below, choose the appropriate order of priorities in the management of a patient with polytruama:
1. Control of extermal haemorrhage
2. Intravenous infusion and transfusion
3. Maintenance of a patient airway
4. Relief of a tension pneumothorax
5. Splinting of fractures
A. 1, 5, 2, 3, 4
B. 3, 4, 1, 2, 5
C. 4, 1, 5, 3, 2
D. 2, 1, 5, 3, 4 - The first step in management of head injury is:
A. Secure airway
B. I.V. mannitol
C. I.V. dexamethasone
D. Blood transfusion - The safest initial approach to open airway of patient with maxillofacial trauma is:
A. Head tilt – chin tilt
B. Jaw thrust technique
C. Head lift – neck lift
D. Heimlich procedure - An average patient with maxillofacial trauma requires how much of daily sodium?
A. 100 mmol
B. 50 – 60 mmol
C. 10 mmol
D. 1000 mmol - Suturing in facial would injuries should be done within:
A. 2 hours
B. 6 hours
C. 4 hours
D. 8 hours - The fracture of the tooth bearing segment of the mandible is:
A. simple
B. complex
C. compound
D. comminuted - Fractures in edentulous mandible are commonly described as:
A. Compound fracture
B. Comminuted fracture
C. Simple fracture
D. Compound comminuted fracture - Of the following which facial bone is most frequently fractured?
A. Mandible
B. Maxilla
C. Nasal
D. Zygomatic - Which side of face is more commonly affected in trauma?
A. Right
B. Left
C. Both equall
D. None - The most common anatomic site of fracture of mandible is the:
A. body
B. angle
C. condyle
D. symphysis - Zygomatic fracture is better viewed in:
A. Reverse town
B. Waters view
C. PA view
D. Submentovertex view
- The radiographic view of choice for demonstrating a nasal # is:
A. Reverse towne’s
B. PA view
C. True lateral
D. OPG - Fracture of mandible all are true except
A. Fractures of the mandible are common at the angle of the mandible.
B. Fractures of the mandible are effected by the muscle pull.
C. Fractures of the mandible are usually characterized by sublingual hematoma.
D. C.S.F. rhinorrhea is a common finding.
- A patient came to the trauma center who had a blow over his lower jaw. Intraoral examination reveals hematoma near lingual side of lower second molar. The proximal fragment is medially displaced. Which of the following might explain the above findings?
A. Vertically favorable fracture of angle of the mandible & displacement is due to masseter action
B. Vertically unfavorable fracture of angle of the mandible & displacement is due to internal pterygoid action
C. Horizontally favourable fracture at the angle & displacement is due to medial pterygoid action
D. Horizontally unfavourable fracture at the angle & displacement is due to masseter action - After a blow to the chin, patient has pain and tenderness over the right TMJ. Open bite, and deviation of the chin to the right side. This suggests:
A. Fracture mandible right angle region
B. Fracture mandible left angle region
C. Fracture mandible right condyle
D. Fracture mandible left condyle - Diagnostic findings of condylar fractures include which of the following:
A. Limitation in opening mouth
B. Evidence of facial trauma, especially in the areaof mandible and symphysis
C. Deviation, upon opening, towards the involved side
D. All of the above
- Early complication following fracture of the mandibular condyle includes all except:
A. Fracture of tympanic plate
B. Vascular injuries
C. Fracture of glenoid fossa with or without displacement of the condylar
segment into the middle cranial fossa
D. Malocclusion
- In which of the following anterior open bite occur?
A. Bilateral condylar fractures
B. Symphysis fracture on one side and angle fracture on the other side of the
mandible
C. Horizontal fracture of the maxilla
D. A & C
- Sixteen-year-old boy presented with pain on left side of the TMJ on mandibular movement. Patient gives H/O road side accident one day back. Clinically, occlusion is normal. Radiograph reveals undisplaced crack in the left mandibular condyle. What is the treatment of choice?
A. Open reduction & internal fixation
B. Maxillo-mandibular fixation for 3 weeks
C. Maxillo-mandibular fixation for 4 weeks
D. No surgical intervention, instruction for soft diet for 3 weeks and observation for any change in occlusion
- Most common complication of condylar injuries in children:
A. Pain
B. Ankylosis
C. Osteoarthritis
D. Fracture of glenoid fossa - In case of subcondylar fracture, the condyle moves in
A. Anterior lateral direction
B. Posterior medial direction
C. Posterior lateral direction
D. Anterior medial direction
- In bilateral parasymphysis fracture the mandible is pulled posteriorly due to the action of
A. Genioglossus
B. Geniohyiod
C. Mylohyoid
D. Hyoglossus - Excessive muscular contraction is one of the frequent cause of:
A. Unilateral condylar fracture
B. Coronoid fracture
C. Fracutre of angle of the mandible
D. Bilateral condylar fracture - Facial widening/flaring is a complication seen in:
A. Symphyseal #
B. Bilateral condylar #
C. Tightening of rnaxillo-mandibular
D. All of the above fixation
- Fracture of body of mandible with full arch of teeth [undisplaced] is treated by
A. IMF
B. Open reduction and internal fixation
C. Close reduction and internal fixation
D. External pin fixation - The treatment for a mandibular fracture between the incisors is treated with
A. Risdon wiring
B. Essig wiring
C. Cap splint with circum-mandibular wiring
D. Transosseous wiring - The ideal treatment for fracture of the angle of mandible is:
A. Transosseous wiring
B. Intermaxillary fixation
C. Plating on the lateral side of the body of the mandible
D. Plating at the inferior border of the mandible
- In condylar fracture with greater than 5 mm overlapping of greater with fracture segment, what is the line of treatment?
A. Closed reduction and IMF
B. ORIF
C. Soft diet
D. No treatment - A Gunning’s splint is used in the treatment of:
A. Fracture of the condyiar neck of a child
B. Fracture of the edentulous mandible
C. Anterior dentoalveolar fracture
D. None of the above - Treatment period of fixation for alveolar bone fracture is
A. 3-4 week
B. 6-8 week
C. 2-3 week
D. 1 week - Important factor in treatment of condylar neck fractures in young patients is by
A. Early mobilization
B. Surgical approach
C. Minibone plating
D. All the above - In children with mixed dentition fracture mandible is treated by:
A. Bone plating
B. Transosseous wiring
C. Eyelet intermaxillary wiring
D. Splinting with circumferential wiring
- After reduction of a mandibular dislocation that occurred for the first time, treatment should be to:
A. Inject sclerosing solution into the joint, so further dislocation is less likely.
B. Inject corticosteroids into the joint which reduces the inflammation.
C. Immobilize with IMF for 5-6 weeks.
D. Advise the patient to limit opening of the mouth for 2-3 weeks.
- Facial paralysis following maxillofacial fractures is most common in
A. # of the condylar neck
B. # of the nasal bones
C. # of the zygomaticomaxillary
D. # of the mandibular symphysis complex. - The inferior orbital fissure is the key to remembering the usual lines of ZMC #, three lines of fracture extend from inferior orbital fissure are:
A. Antero-medial, a supero-medial and lateral direction
B. Antero-medial, a supero-lateral and inferior direction
C. Antero-inferior, a supero-posterior and medial direction
D. Antero-lateral, a supero-lateral and medial direction - Flattening of the cheek seen in:
A. Maxillary fractures
B. Condylar fractures
C. Zygomatic bone fractures
D. Orbital injuries - CSF rhinorrhea is found in:
A. Frontal bone structure
B. Zygomatico maxillary fracture
C. Naso ethmoidal fracture
D. Condylar fracture - The most common site of leak in CSF rhinorrhea is into
A. Sphenoid sinus
B. Frontal sinus
C. Ethmoidal sinus
D. Maxillary sinus - Fracture commonly pyramidal in shape is
A. Le Fort 1
B. Le Fort 2
C. Le Fort3
D. Mandibular - Craniofacial dysjunction seen in
A. Le Fort III fracture
B. Guerrin’s fracture
C. High Le Fort I fracture
D. None of the above - Moon face is seen in:
A. Le Fort I
B. Le Fort II
C. Le Fort III
D. Orbital fractures - Which of the following is not a feature of Le Fort II fracture?
A. Enophthalmos
B. Malocclusion
C. Paraesthesia
D. CSF rhinorrhea - Sub-conjunctival haemorhage occurs due to:
A. Zygomatic complex fractures
B. Orbital fractures
C. Le Fort II fractures
D. All of the above
- The intercanthal distance suggestive of traumatic telecanthus is:
A. 30 mm
B. 32 mm
C. 25 mm
D. 40 mm
- “Dish face’ deformity commonly seen with fractures of middle third of face is because of
A. Posterior and downward movement of maxilla
B. Anterior and forward movement of maxilla
C. Anterior and downward movement of maxilla
D. Nasal complex fracture - Hooding of eyes is seen in which fracture:
A. Le Fort I
B. Le Fort II
C. Le Fort III
D. Nasal bone - Ecchymosis in the post auricular region over the mastoid process is called as
A. Battle’s sign
B. Murphy’s sign
C. Guerin’s sign
D. None - “Hanging drop” sign in the maxillary sinus radiograph usually indicates
A. Nasal bone fracture
B. Orbital floor blow out fracture
C. Isolated coronoid fracture fragment hanging by temporalis muscle
D. Condylar fracture - In blowout fracture of the orbital floor the following occurs
A. Paralysis of lower eyelid
B. Paralysis of upper eyelid
C. Loss of sensation of upper lip
D. None of the above - Diplopia resulting due to facial trauma is all except:
A. Monocular diplopia usually indicates a detached lens, hyphema or other traumatic injuries of globe requiring immediate attention of ophthalmology.
B. Binocular diplopia as a result of trauma due to soft tissue entrapment (muscle or periorbital), neuromuscular injury or a change in orbital shape.
C. General edema of the orbit usually causes diplopia in the extremes of medial or lateral gaze.
D.Diplopia of edema & hemorrhage origin should resolve in a few days, whereas due to entrapment of orbital tissue does not. - Basic mechanism responsible for post traumatic enopthalmos
A. Increase in size of orbit
B. A decrease in content of orbit
C. A disruption in the ligament structure of the globe
D. All of the above
- In blow out fractures which of the following is seen
A. Enophthalmos
B. Exophthalmos
C. Bulbar hemorrhage
D. None - Depressed fracture of the zygomatic area may be clinically recognized by
A. Concavity of the overlying tissue in the zygomatic arch area
B. Interference with movements of the mandible
C. Subluxation of condyles
D. A & B
- During the Gillies approach, the structure of anatomic significance is
A. Superficial temporal artery
B. Marginal mandibular nerve
C. Internal jugular vein
D. Inferior alveolar nerve - Fixation with pack in maxillary sinus is
A. To support comminuted fracture of the body of zygomatic complex
B. To support and reconstitute comminuted orbital floor fracture
C. To protect mucosal covering of maxillary sinus
D. [A] and [B] are correct
- The muscle that aids in displacement of maxillary fractures are:
A. Masseter
B. Temporalis
C. Orbicularis oculi and orbicularis oris
D. None
- Key to successful open reduction of nasal fractures is?
A. Patient presenting before 4 weeks (early treatment)
B. Management of the nasal septum
C. Cartilage segment of septum be handled without resection at all the times
D. All the above - Primary bone healing all are true except:
A. Gap healing and contact healing both produce healed fracture without intermediate cartilaginous callus formation
B. Contact healing is process of bone formation occurring when the interfragmentary gap is essentially zero
C. If the interfragmentary gap is less than 0.5 mm lamellar bone forms directly
D. Primary bone healing relies heavily on periosteum for repair.
- Champy’s plates are?
A. Rigid fixation with bicortical screws
B. Semirigid fixation with monocortical screws
C. Rigid fixation with monocortical screws
D. Semirigid fixation with bicortical screws - Which of them is not rigid osteosynthetic fixation?
A. Osteosynthesis
B. Microplating
C. Screw plating
D. Wiring
- Indication for lag screw osteosynthesis are all except:
A. Fractures in chin region
B. Fractures of the angle
C. Long sagittal fractures in the body region of mandible
D. Short sagittal fracture in the body region of mandible
- In fracture through menta! foramen in atrophic mandible with more than treatment would be
A. Champy’s plate
B. Lag screw
C. Non-rigid fixation
D. Reconstruction plates
- A transverse fracture of symphysis is treated by all of the following except:
A. Two compression plates (2 mm)
B. Two lag screws
C. Single miniplate fixation (1.5 mm)
D. 2.4 mm reconstruction plate - Which of the following provides rigid fixation of the fracture site and heals by primary intention?
A. Direct transosseous wiring
B. Miniplate osteosynthesis without IMF
C. Compression plate osteosynthesis without IMF
D. IMF utilsing arch bars - The treatment of choice in comminuted fracture mandible is?
A. Mini plate
B. External pins
C. Reconstruction plate with central holes
D. Expansive compression plate with screws
- Transosseous wiring is an example of
A. IMF with osteosynthesis
B. Osteosynthesis without IMF
B. IMF
D. None of the above - Compression osteosynthesis heats fracture mandible by
A. Primary union without callus formation
B. Primary union with callus formation
C. Secondary union without callus formation
D. Secondary union with callus formation - Most common complication in mandibular fracture after surgical management is?
A. Witche’s chin
B. Strictures of soft tissue
C. Infection
D. Numbness of area supplied by marginal mandibular - Which of the following is true of non-union of fracture?
A. Mobility of fracture site
B. Bone loss due to infection
C. Early mobilization
D. None of above
- Patient with maxillofacial injuries should be carried in: